A Parents Guide to Iron Deficiency
“…every year there’s always a few athletes who’ve worked hard at practice and in the gym but inevitably hit a wall.”
Why should you care about iron?
As parents we try the best we can to support our kids to get them to practice on-time, eating the healthiest foods (kids are picky eaters), and stay off the phone when it’s time for studying or bed time. As coaches we spend hours analyzing information and attempt to draw up the perfect training plan for each athlete. All of this in hopes that our kids are building healthy habits and in some cases to have a monster sports season that propels them onto the college athletics scene. Despite all of this, every year there’s always a few athletes who’ve worked hard at practice and in the gym but inevitably hit a wall. Initially, confusion sets in for everyone involved but unfortunately after some bloodwork, in most cases we see the culprit is Iron Deficiency (ID). I’m writing this article with the hope that more athletes, coaches and parents in our community read this and are better informed so that ID doesn’t derail months of preparation. After reading this, you should understand more about how iron affects our body and how you can better monitor and address any issues before they become serious.
What is Iron & Why is it Important?
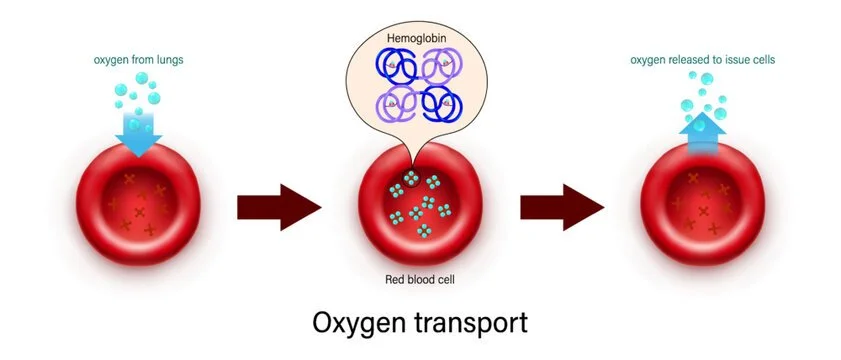
Iron is a fundamental mineral used by the body for numerous processes such as oxygen transport and energy production. Iron binds a protein called transferrin which is essential for the production of special transport proteins called hemoglobin (located on red blood cells in the blood) and myoglobin (within muscle). These transfer proteins shuttle oxygen into the working muscle to fuel exercise and carry carbon dioxide away from the muscles so that exercise can be maintained longer. If iron is in shorty supply the body cannot adequately use oxygen or get rid of waste which prematurely stops the muscle from working optimally. If iron levels become severely low, other factors may be affected which leads to a person being diagnosed with anaemia. Once a person reaches the anaemia stage symptoms are more severe and reversing the condition becomes more difficult, prolonging the recovery time.
Above is a description of how red blood cells combined with hemoglobin shuttle oxygen to target muscles.
Who is at Risk for Iron Deficiency (ID)?
The data suggests that these populations are most at risk for ID :
Females
Blood loss during menstruation and sex-specific hormonal profiles are suspected mechanisms for higher risk.
Iron Deficiency Anaemia (IDA) is estimated to affect 18% of females and 7% of male athletes across a variety of sports (Parks et. At 2017).
Endurance Athletes
Repetitive mechanical nature of the sport is a suspected mechanism for higher risk.
Individuals who have a low energy diet
Vegetarians
Individuals who have chronic gastrointestinal bleeding (i.e. ulcers & hemorrhoids)
Prolonged used of NSAIDs (i.e. aspirin, Advil)
What Are The Signs & Symptoms?
Dizzyness
General weakness and fatigue
Negative mood
Compromised work capacity (not able to perform at typical level)
What Should You Do?
Test Regularly
The first step is to know where you levels are; this means blood tests. Unfortunately, General Practitioners do not always include this in the regular annual physical check-up unless you’re already experiencing symptoms. The good news is if you ask for a test almost all the parents I’ve spoken to have said this is covered under their existing insurance plan.
You should get your blood tested
Annually if you are asymptomatic or have not been diagnosed for ID before.
Quarterly (or bi-annually) if you’re symptomatic or have recently been flagged for low iron levels (within 2-years).
Be sure to get tested for
Ferritin
Hemoglobin (Hb)
Transferrin Saturation
These bio-markers may also be helpful
Serum-Double Transferrin Receptor (sTfR)
Total Iron Binding Capacity (TIBC)
THE IDEAL SITUATION
If possible, create a standardized approach to testing. Because intense exercise and environmental conditions can affect your blood test results, taking blood samples in the morning, >24h post-intense exercise and after an overnight fast (no breakfast) is regarded most optimal. However this is not always possible so try to be as consistent with your blood test prep.
Reading Your Results
Your doctor should go over your results with you, but it’s helpful to have some normal values in mind just in case.
Important : Some results will come back µg/L or ng/ml. Values can be used interchangeably (1 µg/L = 1 ng/ml) .
Ferritin (Mayo Clinic)
(Men) 24 - 336 ug/L
(Women) 11 - 307 ug/L
Hemoglobin [Hb] (LaValle 2013)
(Men) 140-180 g/L
(Women) 120-160 g/L
(Adolescent) 110 - 130 g/L
Transferrin Saturation (University of Rochester)
15 - 50%
Values below 10% may be a signal for anaemia
Serum-Double Transferrin Receptor (sTfR) levels 2.5mg/L
Total Iron Binding Capacity (TIBC) 240-450mcg/dL
Important : Aerobic sport athletes (runners, swimmers, cyclists, etc.) should shoot for levels (ferritin & Hb) closer to the upper end of the reference range.
Stages of Iron Deficiency
Here are some helpful ranges to gauge severity if your results are outside the normative values above.
Stage 1 - Iron Deficiency (ID)
Iron stores in the bone marrow, liver and spleen are depleted (ferritin <35ug/L, Hb > 115g/L, transferrin saturation >16%)
Stage 2 - Iron Deficient Non-Anaemia (IDNA)
Erythropoiesis diminishes as the iron supply to the erythroid marrow is reduced (ferritin <20ug/L, Hb >115 g/L, transferrin saturation <16%)
Stage 3 - Iron-Deficient Anaemia (IDA)
Hb production falls, resulting in anaemia (ferritin <12ug/L, Hb <115 g/L, transferrin saturation <16%).
Important : It’s easier to reverse the incidence of ID in Stage 1 than in the other two stages (IDNA & IDA).
I’m Iron Deficient, Now What?
When faced with ID, there are three primary strategies for supplementation
Increase dietary iron intake (most preferred)
Recommended dietary intake (RDI) is 8mg for males and 18mg for females. However, because athletic populations lose iron through exercise induced mechanisms, it’s important that athletes consume more iron than the normal RDI.
Below are some foods rich in iron, folate and Vitamin B12 that can boost your iron numbers.
Supplemental oral iron (recommended)
Iron supplementation may cause cramping and constipation. Males should consult a doctor before taking. (LaValle)
Slow-release ferrous sulphate remain the established and standard treatment of ID
Vitamin C is considered an iron absorption enhancer so drinking orange juice with your supplement is recommended
Avoid taking iron supplements within an hour before/after drinking coffee
Ask your doctor to recommend a supplement for you.
Intravenous iron supplementation
Using a combination of methods 2 & 3, results can be seen between 8-12 weeks if properly administered. Despite reported rapid improvements using intravenous supplementation, I do not have enough experience to recommend this method. Although not always possible, periods of lower activity (off-season) are great times to maximize iron stores through supplementation
The Food Pantry
Here are some recommendations for foods that are proven to boost red blood cell health which should fuel your comeback.
Foods Rich in Iron
Eggs, Leafy Green Vegetables, Red Meat/Turkey, Lentils/Dry Beans , Nuts (almonds, brazil nuts, cashews), Shellfish (clams & oysters)
Foods Rich in Folate
Eggs, Leafy Green Vegetables, Lentils/Dry Beans, Vegetables (broccoli, cauliflower, string beans, asparagus
Foods Rich in Vitamin B12
Eggs, cheese (Swiss, mozzarella, parmesan), Meat (chicken, beef, turkey), Fish (salmon, tuna, cod), Shellfish (clams & oysters)
Summary
Iron Deficiency (ID) is common and can derail months of hard work.
Some populations are more at risk for ID but can happen to anyone.
Blood tests can give us an inside look at how are body is functioning and if we need to make lifestyle changes.
Iron supplements and dietary considerations can alleviate and reduce the risk of ID & anaemia.
Want to Learn More?
Here are some additional references
Precision Nutrition : Blood Tests & Analysis
Mayo Clinic : Ferritin Test
Your Blood Never Lies : How to Read a Blood Test for a Longer, Healthier Life (LaValle 2013)
University of Rochester Medicine Center : Transferrin
Iron Considerations for the Athlete : A Narrative Review (Sim et al. 2019)